Key Takeaways
-
Awake liposuction is a highly effective, minimally invasive procedure that’s done under local anesthesia. This makes it a feasible option for low-resource clinics around the country in the United States.
-
This technique provides faster recovery and downtime than traditional lipo, benefiting the patients as well as the clinics.
-
Awake lipo is less expensive overall. This allows a greater variety of people to take advantage of body contouring without the expensive fees associated with general anesthesia or hospital admissions.
-
Awake lipo is an entirely outpatient surgery that clinics can perform with minimal medical equipment and with sufficiently trained personnel, lessening the burden on high-resource surgical centers.
-
Patient safety and satisfaction come first with comprehensive pre-op evaluations, rigorous safety measures, and constant communication every step of the way.
-
Having education and training for medical teams is crucial. They ensure optimal standards of care and reproducibly achieve excellent outcomes even in low-resource settings.
Awake lipo in low-resource clinics is a relatively simple procedure that can be done with the patient awake. It’s a procedure that many times uses local numbing rather than general anesthesia. That way, lower-resource clinics with less equipment and lower overhead costs can still provide fat removal for people who want it.
The same can’t be said about U.S. Clinics where awake lipo is actually prevalent—smaller town and busy city aesthetic clinics. It’s cheaper, and patients can return home the same day! Nearly every day, the staff works with minimal tools and makeshift arrangements to ensure safety.
Awake lipo is expanding to settings where funding, equipment, and infrastructure are limited. The following sections will explain the process, what you can do to prepare, and what to expect. This session will focus on safety, regulations, and techniques typically employed in these low-resource clinics.
What Is Awake Liposuction?
Awake liposuction is a type of minimal fat removal procedure that allows the patient to remain awake and aware throughout the entire treatment. Contrary to traditional lipo, which often requires general anesthesia and puts patients under, awake lipo only uses local anesthesia.
This local numbing medicine, usually known as tumescent anesthesia, allows patients to be pain-free and safe. It reduces the amount of anesthetic needed and lets patients remain awake and communicate with the surgical team.
Smaller clinics are increasingly beginning to pick up this technique, particularly in resource-poor areas. It does a great job of saving money and minimizing the risks that come with general anesthesia.

The Basics Explained Simply
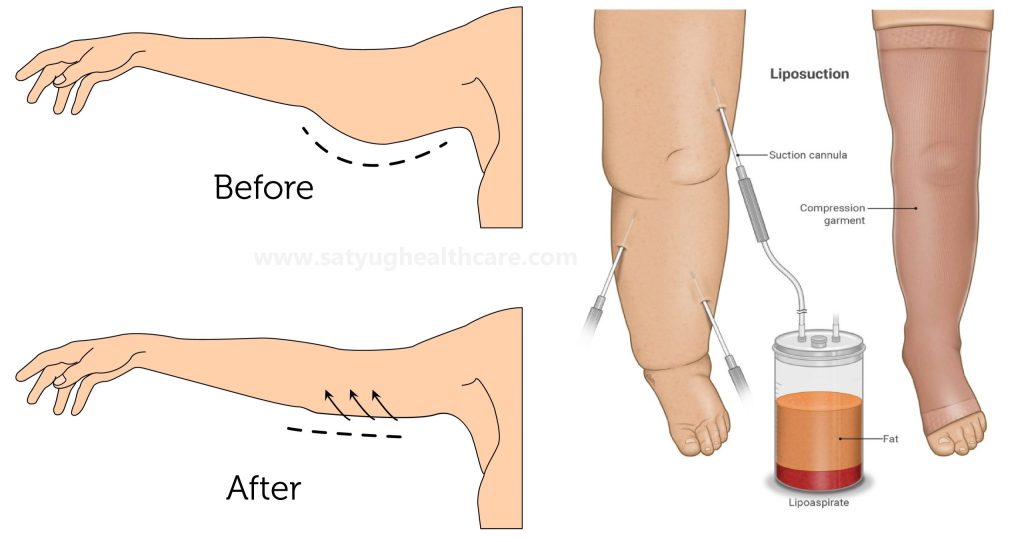
Then, under local anesthesia, the doctor typically begins by marking body areas where excess fat should be removed. Afterward, the space is cleaned and local anesthesia is administered to numb the area.
This solution, called tumescent, swells the tissue. It helps to loosen and take away fat while reducing bleeding and bruising. Next, a thin tube known as a cannula is slid beneath the skin to vacuum up the excess fat.
Typical treatment areas for awake liposuction are the abdomen, inner and outer thighs, flanks, submental (double chin) area and arms. The procedure itself is relatively quick, lasting only 1 to 4 hours depending on how much fat is being removed.
During the procedure, patients are typically engaged in conversation with staff and able to provide real-time feedback, further ensuring comfort and satisfaction.
How It Differs Greatly
Awake liposuction is very different from traditional lipo. The recovery time is often much shorter. Patients report being back on their feet in a few days and back hitting the gym in about a week.
While traditional liposuction often requires a hospital admission, awake lipo can frequently be performed in an outpatient clinic. Your results will continue to improve over the course of a month as swelling subsides.
Though awake lipo offers a safer anesthesia option for more patients, it’s not right for everyone. This technique does have its own risks.
Why Awake Lipo Fits Here
For clinics without extensive resources, awake liposuction presents itself as a more economical option. It provides effective results in body contouring without the expensive laser equipment or complete surgical staff. This technique allows patients to remain awake and, through contracting their muscles, assist the surgeon in identifying the correct areas.
Surgeons can adjust in real-time and notice obvious improvement before the surgery is completed. In cities where budget and space are at a premium, these amenities have significant value.
Making Beauty Affordable
Awake lipo is much more affordable than traditional procedures. It avoids general anesthesia, eliminating the need for expensive anesthesia machines or an elaborate operating room. By creating a network of local clinics, they’re able to minimize overhead and pass the savings directly on to patients.
With costs coming down, more people than ever before are able to experience the remarkable results of body contouring. What’s more, there’s reduced demand for support personnel or extended hospital admission. For instance, a patient in a community-based clinic might pay significantly less for awake lipo than they would for extensive surgery performed at a major hospital.
Less Strain on Clinics
This technique relies on the most rudimentary tools and local anesthesia. Smaller procedures mean that clinics don’t require large operating rooms or highly specialized support. Procedures can go ahead in outpatient procedure rooms, requiring less in the way of supplies, and allowing greater efficiency and availability of more acute care.
Clinics can serve more patients overall, as awake lipo requires a shorter time commitment and less equipment.
Faster Healing, Less Downtime
The majority of patients recover in just a few days. Having only mild soreness or stinging, patients return to work or life in no time. Because awake lipo is less invasive, healing is more seamless.
After a few months, subtle changes begin to take effect as swelling subsides and skin elasticity improves.
Empowering Local Medical Teams
Local surgeons, doctors, and nurses are able to gain awake lipo skills quickly. Along with ensuring quality, the training helps deliver care closer to home and establishes trust in the clinic.
With real-time feedback during surgery, it results in the best possible outcome for each individual patient.
Awake Lipo: Clinic Realities
Awake liposuction is quickly becoming more popular, particularly in cash-strapped clinics. Clinics see it as an answer for body contouring. It lets them skip the higher costs—and higher risks—of using general anesthesia. Patients remain awake, numbing solution is injected, and around 20 minutes later the physician begins to work.
Although patients avoid the hangover of full anesthesia, clinics need to adhere to stringent guidelines to ensure operations remain safe and fluid.
1. Smart Tweaks for Safety
Safety begins well in advance of the first needle. Clinics do often screen patients for risk. They help to make sure people aren’t smoking or drinking in the weeks before surgery as well.
No joke, clean rooms and sterile tools are important. The doctors are in gloves, masks, and gowns, and everything—for lack of a better description—gets wiped down the entire time. A safe endotracheal airway is essential to avoid catastrophic crisis mid-procedure.
While other clinics take shortcuts, just sticking to these fundamentals can reduce risk in a major way.
2. Anesthesia: Safe and Sound
Again, most clinics perform awake lipo without proper anesthesia, using only lidocaine/tumescent anesthesia. That localized numbing really helps minimize any pain during the procedure, and it keeps the patient awake but relaxed.
Other people receive a very low dose of one of these sedatives—maybe Xanax or Valium. An anesthesiologist or nurse monitors patient reactions, and they’re the ones to ensure that patients remain safe and comfortable.
3. Resourceful Equipment Solutions
Adequate suction machines, cannulas, and monitors are non-negotiables. Many low-resource clinics do not have access to the most current tools.
Adoption of modern technology has been shown to improve outcomes and safety. Even rudimentary monitoring equipment such as BP cuffs and pulse oximeters allow one to monitor the patient’s health while a procedure is going on.
4. Training Our Skilled Hands
Training is extremely important. Other providers have as little as a weekend’s worth of instruction, which is dangerous.
Our clinics need to advocate for continued education and hands-on practice, so that staff are aware of the newest techniques.
5. Keeping You Safe Always
Having strong protocols, patient monitoring and quick response plans are critical. Clinics that meet those standards produce the best and safest outcomes for patients and the industry.
Your Lipo Journey Unveiled
Awake liposuction in low-resource clinics offers a pragmatic means of improving access to body contouring. It allows patients to skip lengthy hospital admissions and prolonged recoveries.
It’s much more of a hands-on process than most people realize and patients are very much involved in their own care right from the initial consultation. Setting appropriate expectations and understanding what happens at each step can go a long way toward improving outcomes and your overall satisfaction with the process.
Getting Ready: First Steps
Before awake lipo, patients should:
-
Stop certain medications (like blood thinners) as advised.
-
Avoid smoking and alcohol for at least a week.
-
Arrange for a ride home after the procedure.
-
Wear loose, comfy clothes on procedure day.
An in-depth medical history review is essential. This assists in identifying potential health risks and allows the clinic to be prepared to give you the best care possible.
It’s important for patients to be open about what they want to achieve and express any concerns they have with their surgeon as well. This helps form a strategy that addresses their specific needs and mitigates risk while ensuring all parties are aligned.
During Your Awake Lipo
During the procedure you can look forward to being awake but comfortable. The lipo area is solely numbed with a local anesthesia and the lipo team is constantly checking in with you to ensure a comfortable experience.
The entire process is generally 1 to 4 hours, depending on the number of areas being treated. This arrangement allows patients to engage in conversation with staff, adding a level of comfort that helps calm apprehensions while increasing feelings of empowerment.
Gentle suction and other small techniques reduce pain and swelling.
After: Healing and Care
Post-op care tips:
-
Wear a compression garment for about 6 weeks.
-
For 2 weeks after surgery, we recommend wearing foam pads underneath the compression garment.
-
Stay active, but skip hard exercise for a while.
-
Keep the treated area clean and dry.
The average return to work is one week. Soreness and drainage from the incision are normal and will disappear within a few weeks.
Expect swelling for 4-6 weeks; full results will appear in several months. Continued post-operative follow-up is imperative for monitoring healing and ongoing outcomes.
Seeing is Believing: Results
Awake liposuction offers an alternative approach to body contouring, particularly in resource-poor settings. Results are different for everyone. Those can be the shape of the body, the skill of the physician, and the configuration of the clinic. Others experience a visible reduction in shape after just 24 hours!
Some people may require several weeks for the swelling to subside and the outcomes to appear. These are all expected changes to continue occurring as the body heals.
What Changes Can You Expect?
The majority of individuals observe improved smoothness and reduced plumpness in the treated areas. Hips, thighs, belly, and arms take on a curvy silhouette. Results vary based on the physician’s expertise, the volume of fat removed, and the treatment areas on the body.
Awake lipo is typically performed under local anesthesia on three or fewer body areas at a time, so dramatic, full-body transformations are not realistic. Maintaining positive lifestyle changes post-op, such as a healthy diet and exercise, are vital for maintaining long-lasting results.
Even these outcomes aren’t always gold. Sometimes fat doesn’t come off evenly or doesn’t quite match your vision. This is usually the case when the clinic’s equipment or expertise is lacking.
Real Stories, Real Smiles
Patients who have transitioned from low-resource clinics tell us how their lives have changed and their spirits lifted after awake lipo. They share stories about jeans fitting better or not being self-conscious at the pool.
However, people don’t seem to be happy across the board—some complain of pain while undergoing the procedure or inconsistent results that didn’t achieve the desired evenness. Seeing others excited about their transformations can go a long way in educating folks about what’s possible.
Setting Realistic Goals
Communicating everything with an experienced surgeon is critical. It both forces you to create a clear vision of what you want and helps manage people’s expectations. Some believe awake lipo can’t compare to the original variety, but many others agree that the results come pretty darn close.
Education goes a long way to make patients discerning consumers and able to cut through the hype. When goals are misaligned, poor outcomes or increased expenses later on are inevitable. If the process is done poorly, those problems will repeat themselves.
Navigating Hurdles in Care
Providing awake liposuction in low-resource clinics comes with a different set of hurdles that extend beyond the initial lack of resources available. Continuing to put patient safety first requires navigating these constraints while continuing to adhere to the principles of high quality care.
Clinics face liabilities such as hypothermia when extensive areas of skin are exposed and cold fluids are utilized. Long operative and procedure times further compound those risks, particularly where the quality of monitoring equipment may not be state-of-the-art. Monitoring vital signs—such as central venous pressure, arterial blood pressure, and urine output—is key. That’s really hard to do when the resources just aren’t there.
Flexibility is key on the ground. Most clinics adjust their protocols, such as pre-warming all fluids before administration or streamlining procedures to minimize time. Given limited budgets, staff have to get imaginative, relying on checklists and low-tech tracking tools to compensate for what’s often a lack of thorough equipment.
Patient education is huge. Teach patients what to expect, including which medications to discontinue—like statins or calcium channel blockers. Provide a rationale for ordering a test such as a complete blood count or liver function panel to assist in avoiding complications.
Making Most of Less
-
Warm fluids before use and limit procedure time.
-
Use checklists for pre-op tests and meds review.
-
Rely on teamwork to catch early warning signs.
-
Set up simple systems for tracking fluids and vitals.
Interprofessional collaboration between nursing, anesthesia, and surgery allows for proactive identification of issues. Local volunteers or partners may be able to assist with providing or obtaining needed supplies or providing support for patients.
Local Rules and You
Staying up-to-date with local health regulations protects clinics, their patients, and the communities they serve. Each locality might have different forms or requirements that you’ll need to address.
Having an understanding of these rules from the beginning will prevent clinics from facing potentially crippling fines or even shut-downs.
Understanding Local Views
Cosmetic surgery still has a certain stigma attached. Clinics should consider hosting information sessions or Q&A forums to address concerns.
Clear dialogue around risks and benefits fosters trust, helping the community accept awake lipo.
Conclusion
Awake lipo delivers a genuine opportunity for safe body shaping for people in low-resource clinics. The approach avoids big pharmaceuticals and big equipment. In this way, more patients get high-quality care without a hefty cost or extensive delays. Staff catch on fast, and patients recuperate quickly. Clinics can do less and still produce good outcomes. It’s not magic, but it carries serious influence where budgets are limited. Real people in real places have an honest shot at making a difference, right where they live and work. If you’re interested, inquire about it at your local clinic or speak with someone who has had it performed. Stay informed, stay accurate, and above all, stay healthy. Proper decisions place you in a better position for the future.
Frequently Asked Questions
What is awake liposuction?
What is awake liposuction? Being awake and alert during the procedure allows for a quicker recovery time and reduces risks.
Why is awake lipo suitable for low-resource clinics?
Awake lipo requires less equipment and fewer staff members compared with a traditional surgery. It’s safer, more affordable and aligns with the capacity of low-resource clinics.
Is awake lipo safe in low-resource settings?
Yes, as long as it is done by trained and qualified professionals with sterile equipment, awake lipo is safe. General anesthesia carries a higher risk of complication compared to local anesthesia.
How long does recovery take after awake lipo?
Patients are usually back to light activity in a matter of days. Complete recovery typically takes around two weeks, though this varies based on your overall health and the area you have treated.
What should I expect during my awake lipo journey?
You’ll receive a local anesthetic, remain awake during the procedure, and experience only minimal discomfort. You’ll find some procedures only take a few hours and you may be able to go home the same day.
Will I see results right away?
While you will start to see a difference almost immediately after your procedure, swelling can hide results. Final results typically show within a few weeks as your body recovers.
What are the most common hurdles in awake lipo care?
What are the most common hurdles in awake lipo care. Selecting an experienced clinic with high safety standards to address individual needs is the best way to move forward.